Healthcare Revenue Cycle Management Market Overview
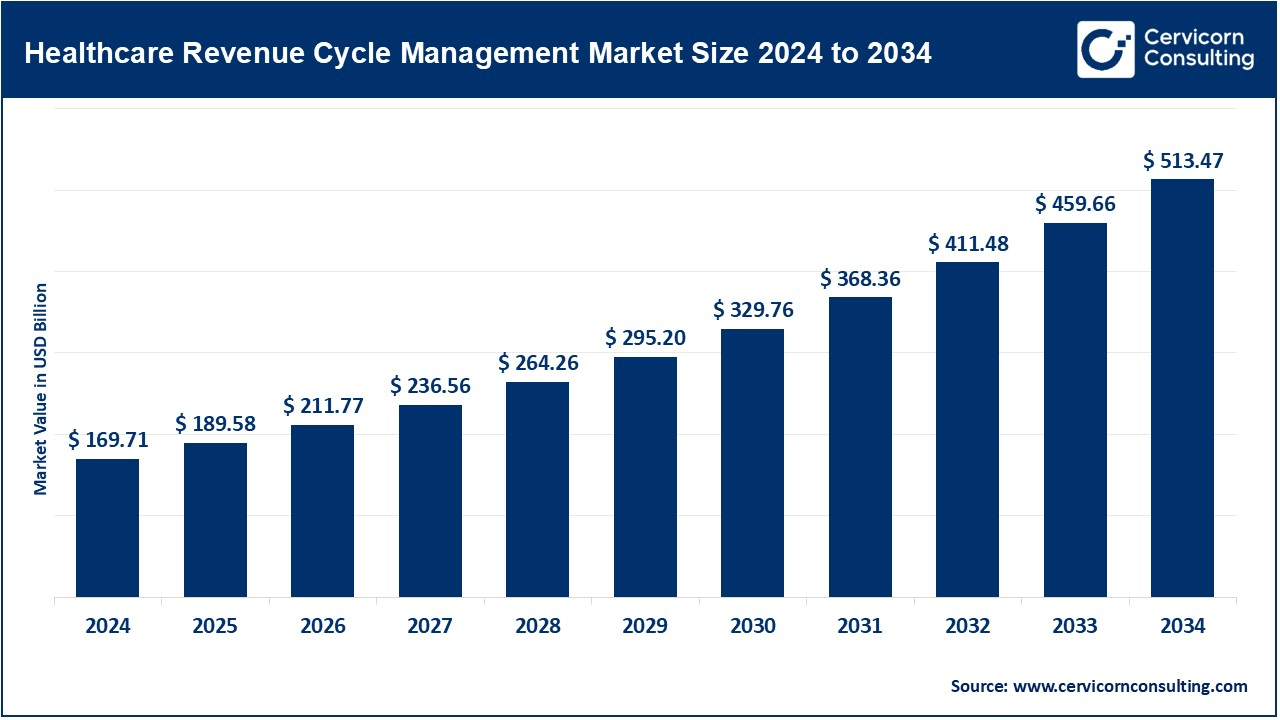
The global healthcare revenue cycle management (RCM) market was valued at approximately USD 169.71 billion in 2024 and is projected to grow to around USD 513.47 billion by 2034, exhibiting a CAGR of 11.70% from 2025 to 2034. RCM encompasses the entire financial workflow of healthcare providers, covering patient registration, medical coding, claims submission, denial management, and payment collection. Market expansion is being fueled by rising healthcare spending, increasing patient volumes, digital transformation, and the adoption of automation technologies aimed at improving operational efficiency and optimizing revenue capture.
Key Market Trends
1. Integration of AI and Automation
Artificial intelligence (AI) and machine learning (ML) are being increasingly incorporated into RCM processes. These technologies enable automated claims validation, predictive denial management, smart coding, and revenue analytics, significantly reducing manual effort and accelerating reimbursement cycles. For example, AI-driven denial prediction systems allow healthcare providers to identify and address potential claim rejections before submission, reducing revenue leakage.
2. Cloud-Based and SaaS RCM Solutions
There is a clear trend toward migrating from traditional on-premise RCM platforms to cloud-based and Software-as-a-Service (SaaS) solutions. Cloud adoption facilitates real-time analytics, scalability, and cost-effective deployment while supporting multi-location and remote operations—an ideal setup for large hospitals and multi-specialty practices.
3. EHR-RCM Interoperability
Seamless integration between Electronic Health Records (EHRs) and RCM systems is becoming increasingly vital. Such integration ensures accurate clinical-to-financial workflow mapping, minimizes billing errors, and enhances operational efficiency across hospitals, clinics, and ambulatory care networks.
4. Patient-Centric Billing and Engagement
As patients bear a greater share of healthcare costs (co-pays, deductibles), providers are focusing on transparent billing, digital payment portals, and automated reminders. Patient-centric billing improves collection rates, reduces disputes, and enhances overall patient satisfaction.
5. Regulatory Compliance and Data Security
Stricter regulations, such as HIPAA and regional privacy standards, are driving RCM vendors to adopt secure architectures, immutable audit trails, and compliance-ready workflows. These solutions help healthcare organizations minimize legal risks while maintaining financial integrity.
Get a Free Sample: https://www.cervicornconsulting.com/sample/2598
Market Drivers
-
Rising Healthcare Costs and Utilization: Increasing per-capita healthcare spending and higher patient volumes are driving demand for efficient revenue management systems.
-
Digital Transformation: Adoption of cloud computing, AI, and automation is enhancing the functionality and accessibility of RCM platforms.
-
Operational Efficiency and Cost Reduction: Automated workflows reduce administrative overhead, improve claim accuracy, and accelerate cash flow.
-
Shift to Value-Based Care: Performance-based reimbursement models require tracking outcomes and reconciling complex claims, boosting demand for sophisticated RCM solutions.
-
Telehealth Expansion: The rise of virtual care introduces new billing complexities, encouraging adoption of cloud-based and automated RCM platforms.
Impact of Trends and Drivers
-
Hospitals and Health Systems: Adoption of integrated RCM systems reduces denial rates, revenue leakage, and days in accounts receivable, improving overall financial performance.
-
Physician Practices and Ambulatory Care: Smaller providers leverage cloud-based or outsourced RCM solutions to access enterprise-level functionality without high upfront costs.
-
Regional Dynamics: North America dominates the market due to advanced EHR adoption and strict regulatory compliance, while Asia-Pacific is the fastest-growing region, driven by investments in digital healthcare infrastructure.
-
Managed Service Providers (MSPs): Outsourcing of RCM functions allows smaller organizations to access advanced technology and reduce operational expenses.
Challenges and Opportunities
Challenges
-
Integrating legacy EHR systems with modern RCM platforms can be complex and resource-intensive.
-
Compliance with multi-jurisdictional privacy and healthcare regulations poses ongoing hurdles.
-
Staff training and change management are necessary as automation replaces manual processes.
Opportunities
-
AI-powered denial prevention and predictive collections enhance operational efficiency.
-
Expansion of cloud and outsourced RCM services offers access to small and mid-sized practices.
-
Development of specialty-specific RCM platforms for oncology, behavioral health, and telehealth presents new growth avenues.
Future Outlook
The healthcare RCM market is set to sustain robust growth, reaching an estimated USD 513.47 billion by 2034, with a CAGR of 11.70%. Future solutions will increasingly be cloud-first, AI-driven, and patient-centric, supporting interoperability, compliance, and automation. North America will maintain its position as the largest market, while Asia-Pacific is expected to emerge as the fastest-growing region. Providers and vendors that prioritize integration, compliance, and advanced automation will capture the largest share of this expanding and evolving market.
For a detailed market overview or company-specific insights, contact: Cervicorn Consulting